Abstract
BTK inhibitors deeply affect the proliferative capacity, homing and migrations of chronic lymphocytic leukemia (CLL) cells, and cause their redistribution from nodal compartments to the blood stream. Reciprocal expression of CXCR4 and CD5 on circulating CLL cells is an established marker discriminating the proliferative fraction (CD5high/CXCR4dim, PF), recently egressed from the lymph node, from the resting fraction (CXCR4high/CD5dim, RF) of older, quiescent cells navigating the blood stream.
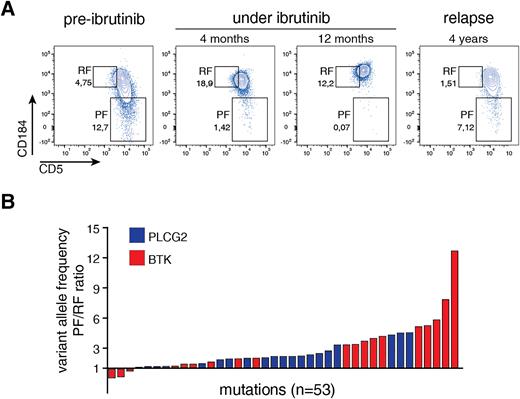
We monitored the dynamics of the PF under the course of ibrutinib therapy in 31 CLL cases recruited in the IOSI-EMA-001 study (NCT02827617) with sequential blood sampling (156 samples, median 6 samples/case, range 3-7). PF was monitored through fixed gates, designed on the pre-treatment sample around the population visually detaching from the main cluster (panel A). Longitudinal analysis showed a depletion of the PF over time, from a median of 17.7% at pre-treatment to 4.75, 0.4, 1.5, 0.6, 1.5% at subsequent timepoints (0.5, 6, 12, 18, 24 months; range 0-50; p < 0.001, U test). Loss of proliferative potential was confirmed by concurrent loss of Ki67 expression.
We retrospectively analyzed the PF from a second cohort of 99 ibrutinib-treated CLL cases from the real world, referred for routine immunophenotyping (278 samples, median 3 samples/case, range 2-7). Median PF of pre-ibrutinib samples was 12.0% (range 0.7-50%), with a significant drop to 2.7% after 1 year of treatment and to 1.0% after 2 years (p<0.001, U test). Out of 99 cases, 55 discontinued ibrutinib within 5 years (16 toxicity, 38 progression/relapse, 1 death; median time of treatment 29.7 months, range 1-58.6 months). Median PF in samples collected after ibrutinib discontinuation was 1.15% after 2 years of treatment, and increased to 13.3, 7.10, 6.30, 12.0% after 3, 4, 5 and >5 years. Conversely, samples collected under ibrutinib treatment presented a more stable trend of median PF (3.0 and 3.5% after 3 and 4 years respectively). Interestingly, of 27 patients with blood samples collected during the third year of therapy, 11 failed ibrutinib due to relapse/progression within the following two years: these cases presented a higher median PF (10.0%) than cases who stayed on ibrutinib (median PF 1.8%, p=0.045). Mutations of BTK/PLCG2 were detected in 28/99 cases (28.2%); among these, 18 (64.2%) discontinued ibrutinib due to progression/relapse (17/18) or toxicity (1/18), whereas 10 cases, although mutated, remained on treatment. Median time of appearance of BTK/PLCG2 mutations was 48 months (range 16-70). Median VAF was 22.8 (range 1.2-99.0) and 3.5 (range 1.7-17.6) for BTK and PLCG2, respectively.
We isolated the PF and RF fractions from 10 cases developing BTK/PLCG2 mutations, who showed reappearance of the PF after prolonged ibrutinib treatment (median 50.7 months). Sequencing revealed 1.7 mean BTK mutations per sample (range 1-4), with a median VAF higher in the PF (23.0%, range 0.3-92.3) than in the RF (5.15%, range 0.1-84.8; p=0.0027, paired rank test); overall, the PF VAF was almost 3 times larger than the RF (average 2.82, range 0.01-38). Accompanying PLCG2 mutations were present in 6 cases, generally more frequent (average 3.7 mutations per case, range 1-8) but with lower burden (median VAF 1.7%, range 0.1-4.3) than BTK mutations; again, average the PF fraction had higher VAF than the RF (average PF: 2.0, range 0.1-6.2; average RF: 1.35, range 0.4-2.8; p=0.0142) (panel B).
Finally, we performed mRNA-seq on 6 cases relapsed after ibrutinib, isolating the RF and the newly reconstituted PF, the latter enriched in BTK mutations, with matching fractions isolated from pre-ibrutinib samples. Differential expression signature of PF vs. RF at pre-treatment was concordant with published gene sets (e.g. Calissano et al. Mol Med 2011); application of this signature to post-ibrutinib PF/RF fractions drove co-clustering of 12 out of 13 fractions with their respective pre-treatment counterparts, suggesting that the reconstituted PF fraction at relapse is functionally similar to the original pre-treatment PF. Overall, our data support the hypothesis that, in patients undergoing ibrutinib treatment, BTK/PLCG2 mutations arise within the lymph nodes, the proliferative compartment of CLL; clinically, longitudinal monitoring of the CXCR4/CD5 fractions by flow cytometry may provide a simple tool helping to intercept CLL progression under ibrutinib therapy.
Disclosures
Rossi:BeiGene: Consultancy, Honoraria, Other: Travel Support, Research Funding; AbbVie: Consultancy, Honoraria, Other: Travel Support, Research Funding; Janssen: Consultancy, Honoraria, Other: Travel Support, Research Funding; Gilead: Other: honoraria, advisory board fees , Research Funding; MSD: Other: advisory board fees ; AstraZeneca: Consultancy, Honoraria, Other: Travel Support, Research Funding; BMS: Consultancy, Honoraria, Other: Travel Support.
Author notes
Asterisk with author names denotes non-ASH members.